All About Achilles Tendinitis
16/12/2014 17:45
Overview
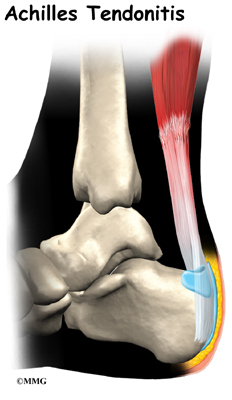 Achilles tendonitis is one of the most common running injuries. The achilles tendon is the large tendon at the back of the ankle. It connects the calf muscles made up of the gastrocnemius and soleus to the heel bone or calcaneus. It provides the power in the push off phase of walking and running where huge forces are transmitted through the achilles tendon. Achilles tendonitis is often now referred to as achilles tendinopathy. This is because the term tendinopathy covers all types of overuse achilles tendon injury. Strictly speaking tendonitis suggests an inflammatory condition of the tendon but in reality few achilles tendon injuries are actually down to pure inflammation. Soleus muscleThe main finding, particularly in older athletes is usually degeneration of the tissue with a loss of normal fibre structure. Other very similar conditions may actually be due to inflammation or degeneration of the tendon sheath which surrounds the tendon rather than the achilles tendon itself. In addition to being either chronic or acute, achilles tendonitis can also be at the attachment point to the heel called insertional achilles tendonitis or in the mid-portion of the tendon typically around 4cm above the heel. Healing of the achilles tendon is often slow, due to its poor blood supply.
Achilles tendonitis is one of the most common running injuries. The achilles tendon is the large tendon at the back of the ankle. It connects the calf muscles made up of the gastrocnemius and soleus to the heel bone or calcaneus. It provides the power in the push off phase of walking and running where huge forces are transmitted through the achilles tendon. Achilles tendonitis is often now referred to as achilles tendinopathy. This is because the term tendinopathy covers all types of overuse achilles tendon injury. Strictly speaking tendonitis suggests an inflammatory condition of the tendon but in reality few achilles tendon injuries are actually down to pure inflammation. Soleus muscleThe main finding, particularly in older athletes is usually degeneration of the tissue with a loss of normal fibre structure. Other very similar conditions may actually be due to inflammation or degeneration of the tendon sheath which surrounds the tendon rather than the achilles tendon itself. In addition to being either chronic or acute, achilles tendonitis can also be at the attachment point to the heel called insertional achilles tendonitis or in the mid-portion of the tendon typically around 4cm above the heel. Healing of the achilles tendon is often slow, due to its poor blood supply.
Causes
Tight or tired calf muscles, which transfer too much of the force associated with running onto the Achilles tendon. Not stretching the calves properly or a rapid increase in intensity and frequency of sport training can make calf muscles fatigued. Activities which place a lot of stress on the achilles tendon, such as hill running and sprint training, can also cause Achilles Tendinitis. Runners who overpronate (roll too far inward on their feet during impact) are most susceptible to Achilles Tendinitis. Runners with flat feet are susceptible to Achilles Tendinitis because flat feet cause a 'wringing out' effect on the achilles tendon during running. High arched feet usually absorb less shock from the impact of running so that shock is transferred to the Achilles tendon. Use of inappropriate footwear when playing sport or running e.g., sandals, can also put an extra load on the Achilles tendon. Shoes are now available that have been designed for individual sports and provide cushioning to absorb the shock of impact and support for the foot during forceful movements. Training on hard surfaces e.g., concrete, also increases the risk of Achilles Tendinitis. Landing heavily or continuously on a hard surface can send a shock through the body which is partly absorbed by the Achilles tendon. A soft surface like grass turf helps to lessen the shock of the impact by absorbing some of the force of the feet landing heavily on the ground after a jump or during a running motion.
Symptoms
Mild ache in the back of the lower leg, especially after running. More acute pain may occur after prolonged activity, Tenderness or stiffness in the morning. In most cases the pain associated with Achilles tendinitis is more annoying than debilitating, making sufferers regret activity after the fact, but not keeping them from doing it. More severe pain around the Achilles tendon may be a symptom of a much more serious ruptured tendon.
Diagnosis
Studies such as x-rays and MRIs are not usually needed to make the diagnosis of tendonitis. While they are not needed for diagnosis of tendonitis, x-rays may be performed to ensure there is no other problem, such as a fracture, that could be causing the symptoms of pain and swelling. X-rays may show evidence of swelling around the tendon. MRIs are also good tests identify swelling, and will show evidence of tendonitis. However, these tests are not usually needed to confirm the diagnosis; MRIs are usually only performed if there is a suspicion of another problem that could be causing the symptoms. Once the diagnosis of tendonitis is confirmed, the next step is to proceed with appropriate treatment. Treatment depends on the specific type of tendonitis. Once the specific diagnosis is confirmed, the appropriate treatment of tendonitis can be initiated.
Nonsurgical Treatment
Most of the time, treatment for achilles tendinitis beginning with nonsurgical options. Your CFO physician may recommend rest, ice, ibuprofen, and physical therapy. If after 6 months, the pain does not improve, surgical treatment may be necessary. The type of surgery would depend on the exact location of the tendinitis and extent of damage.

Surgical Treatment
For paratenonitis, a technique called brisement is an option. Local anesthetic is injected into the space between the tendon and its surrounding sheath to break up scar tissue. This can be beneficial in earlier stages of the problem 30 to 50 percent of the time, but may need to be repeated two to three times. Surgery consists of cutting out the surrounding thickened and scarred sheath. The tendon itself is also explored and any split tears within the tendon are repaired. Motion is started almost immediately to prevent repeat scarring of the tendon to the sheath and overlying soft tissue, and weight-bearing should follow as soon as pain and swelling permit, usually less than one to two weeks. Return to competitive activity takes three to six months. Since tendinosis involves changes in the substance of the tendon, brisement is of no benefit. Surgery consists of cutting out scar tissue and calcification deposits within the tendon. Abnormal tissue is excised until tissue with normal appearance appears. The tendon is then repaired with suture. In older patients or when more than 50 percent of the tendon is removed, one of the other tendons at the back of the ankle is transferred to the heel bone to assist the Achilles tendon with strength as well as provide better blood supply to this area.
Prevention
Warm up slowly by running at least one minute per mile slower than your usual pace for the first mile. Running backwards during your first mile is also a very effective way to warm up the Achilles, because doing so produces a gentle eccentric load that acts to strengthen the tendon. Runners should also avoid making sudden changes in mileage, and they should be particularly careful when wearing racing flats, as these shoes produce very rapid rates of pronation that increase the risk of Achilles tendon injury. If you have a tendency to be stiff, spend extra time stretching. If you?re overly flexible, perform eccentric load exercises preventively. Lastly, it is always important to control biomechanical alignment issues, either with proper running shoes and if necessary, stock or custom orthotics.
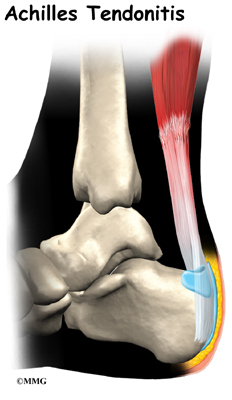 Achilles tendonitis is one of the most common running injuries. The achilles tendon is the large tendon at the back of the ankle. It connects the calf muscles made up of the gastrocnemius and soleus to the heel bone or calcaneus. It provides the power in the push off phase of walking and running where huge forces are transmitted through the achilles tendon. Achilles tendonitis is often now referred to as achilles tendinopathy. This is because the term tendinopathy covers all types of overuse achilles tendon injury. Strictly speaking tendonitis suggests an inflammatory condition of the tendon but in reality few achilles tendon injuries are actually down to pure inflammation. Soleus muscleThe main finding, particularly in older athletes is usually degeneration of the tissue with a loss of normal fibre structure. Other very similar conditions may actually be due to inflammation or degeneration of the tendon sheath which surrounds the tendon rather than the achilles tendon itself. In addition to being either chronic or acute, achilles tendonitis can also be at the attachment point to the heel called insertional achilles tendonitis or in the mid-portion of the tendon typically around 4cm above the heel. Healing of the achilles tendon is often slow, due to its poor blood supply.
Achilles tendonitis is one of the most common running injuries. The achilles tendon is the large tendon at the back of the ankle. It connects the calf muscles made up of the gastrocnemius and soleus to the heel bone or calcaneus. It provides the power in the push off phase of walking and running where huge forces are transmitted through the achilles tendon. Achilles tendonitis is often now referred to as achilles tendinopathy. This is because the term tendinopathy covers all types of overuse achilles tendon injury. Strictly speaking tendonitis suggests an inflammatory condition of the tendon but in reality few achilles tendon injuries are actually down to pure inflammation. Soleus muscleThe main finding, particularly in older athletes is usually degeneration of the tissue with a loss of normal fibre structure. Other very similar conditions may actually be due to inflammation or degeneration of the tendon sheath which surrounds the tendon rather than the achilles tendon itself. In addition to being either chronic or acute, achilles tendonitis can also be at the attachment point to the heel called insertional achilles tendonitis or in the mid-portion of the tendon typically around 4cm above the heel. Healing of the achilles tendon is often slow, due to its poor blood supply.
Causes
Tight or tired calf muscles, which transfer too much of the force associated with running onto the Achilles tendon. Not stretching the calves properly or a rapid increase in intensity and frequency of sport training can make calf muscles fatigued. Activities which place a lot of stress on the achilles tendon, such as hill running and sprint training, can also cause Achilles Tendinitis. Runners who overpronate (roll too far inward on their feet during impact) are most susceptible to Achilles Tendinitis. Runners with flat feet are susceptible to Achilles Tendinitis because flat feet cause a 'wringing out' effect on the achilles tendon during running. High arched feet usually absorb less shock from the impact of running so that shock is transferred to the Achilles tendon. Use of inappropriate footwear when playing sport or running e.g., sandals, can also put an extra load on the Achilles tendon. Shoes are now available that have been designed for individual sports and provide cushioning to absorb the shock of impact and support for the foot during forceful movements. Training on hard surfaces e.g., concrete, also increases the risk of Achilles Tendinitis. Landing heavily or continuously on a hard surface can send a shock through the body which is partly absorbed by the Achilles tendon. A soft surface like grass turf helps to lessen the shock of the impact by absorbing some of the force of the feet landing heavily on the ground after a jump or during a running motion.
Symptoms
Mild ache in the back of the lower leg, especially after running. More acute pain may occur after prolonged activity, Tenderness or stiffness in the morning. In most cases the pain associated with Achilles tendinitis is more annoying than debilitating, making sufferers regret activity after the fact, but not keeping them from doing it. More severe pain around the Achilles tendon may be a symptom of a much more serious ruptured tendon.
Diagnosis
Studies such as x-rays and MRIs are not usually needed to make the diagnosis of tendonitis. While they are not needed for diagnosis of tendonitis, x-rays may be performed to ensure there is no other problem, such as a fracture, that could be causing the symptoms of pain and swelling. X-rays may show evidence of swelling around the tendon. MRIs are also good tests identify swelling, and will show evidence of tendonitis. However, these tests are not usually needed to confirm the diagnosis; MRIs are usually only performed if there is a suspicion of another problem that could be causing the symptoms. Once the diagnosis of tendonitis is confirmed, the next step is to proceed with appropriate treatment. Treatment depends on the specific type of tendonitis. Once the specific diagnosis is confirmed, the appropriate treatment of tendonitis can be initiated.
Nonsurgical Treatment
Most of the time, treatment for achilles tendinitis beginning with nonsurgical options. Your CFO physician may recommend rest, ice, ibuprofen, and physical therapy. If after 6 months, the pain does not improve, surgical treatment may be necessary. The type of surgery would depend on the exact location of the tendinitis and extent of damage.

Surgical Treatment
For paratenonitis, a technique called brisement is an option. Local anesthetic is injected into the space between the tendon and its surrounding sheath to break up scar tissue. This can be beneficial in earlier stages of the problem 30 to 50 percent of the time, but may need to be repeated two to three times. Surgery consists of cutting out the surrounding thickened and scarred sheath. The tendon itself is also explored and any split tears within the tendon are repaired. Motion is started almost immediately to prevent repeat scarring of the tendon to the sheath and overlying soft tissue, and weight-bearing should follow as soon as pain and swelling permit, usually less than one to two weeks. Return to competitive activity takes three to six months. Since tendinosis involves changes in the substance of the tendon, brisement is of no benefit. Surgery consists of cutting out scar tissue and calcification deposits within the tendon. Abnormal tissue is excised until tissue with normal appearance appears. The tendon is then repaired with suture. In older patients or when more than 50 percent of the tendon is removed, one of the other tendons at the back of the ankle is transferred to the heel bone to assist the Achilles tendon with strength as well as provide better blood supply to this area.
Prevention
Warm up slowly by running at least one minute per mile slower than your usual pace for the first mile. Running backwards during your first mile is also a very effective way to warm up the Achilles, because doing so produces a gentle eccentric load that acts to strengthen the tendon. Runners should also avoid making sudden changes in mileage, and they should be particularly careful when wearing racing flats, as these shoes produce very rapid rates of pronation that increase the risk of Achilles tendon injury. If you have a tendency to be stiff, spend extra time stretching. If you?re overly flexible, perform eccentric load exercises preventively. Lastly, it is always important to control biomechanical alignment issues, either with proper running shoes and if necessary, stock or custom orthotics.
Contact
Carmella Buchsbaum
r02360809851303@hotmail.com
